Introduction: Heparin is used for both therapeutic anticoagulation and thromboprophylaxis in admitted with COVID-19. However, multiple studies have shown an increased risk of heparin induced thrombocytopenia (HIT) among hospitalized patients with COVID-19. We conducted a large nationwide study to determine the impact of HIT on hospitalization outcomes among patients with COVID-19.
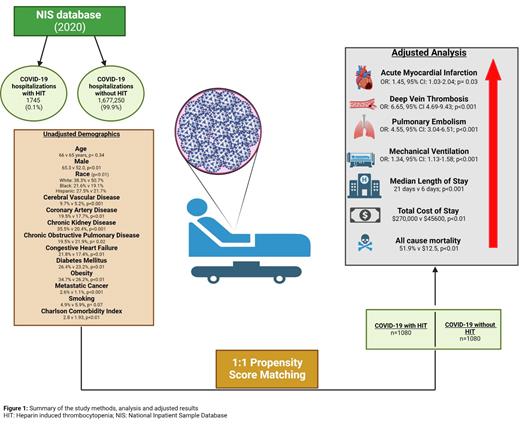
Methods: The National Inpatient Sample Database (NIS) was interrogated using the appropriate International Classification of Diseases (1CD) 10 codes to determine hospitalizations for COVID-19 in 2020. The Data was then subclassified into cases with and without HIT. Chi square test and Mann Whitney U test were used to compare categorical and continuous variables, respectively. Subsequently, 1:1 propensity score matching (PSM) using the nearest neighbor with a match tolerance of zero was performed to match the two groups for patient demographics, and comorbidities. The primary endpoint was the difference in all-cause mortality. Other secondary endpoints included common hospitalization complications like acute myocardial infarction (AMI), deep vein thrombosis (DVT), pulmonary embolism (PE), and respiratory failure requiring mechanical ventilation (MV). We also performed a cost analysis to determine the differences in cost and length of stay. A p value of <0.05 was considered significant. All statistical methods were performed using SPSS Version 28.0.
Results: A total of 1,678,995 weighted hospitalizations for COVID-19 were recorded in 2020. Among these 1745 (0.1%) had concurrent HIT. COVID-19 patients with HIT were more likely to be male (65.3% vs 52.0; p<0.01) and black (21.6% vs 19.1%, p<0.01). More patients with HIT had comorbid conditions compared to patients without HIT, most notably history of cerebrovascular disease (9.7% vs 5.2%), chronic kidney disease (35.5% vs 20.4%), congestive heart failure (21.8% vs 17.4%), diabetes mellitus (26.4% vs 23.2%), metastatic cancer (2.6% vs 1.1%), and obesity (34.7% vs 26.2%) (all p<0.01). PSM was used to match 1080 cases with HIT to 1080 without HIT. Hospitalizations with HIT had higher odds of all-cause mortality (Odds Ratio [OR] = 7.54, 95% confidence interval [CI]: 6.07-9.36; p<0.01). Patients with HIT also had higher odds of AMI (OR = 1.45, 95% CI: 1.03-2.04; p<0.01), DVT (OR = 6.65, 95% CI: 4.69-9.42; p<0.01), PE (OR = 4.45, 95% CI: 3.04-6.51, p<0.01), and MV (OR = 12.66, 95% CI: 10.22-15.69; p<0.01). COVID-19 patients with HIT also had a higher median LOS (21.0 vs 6.00 days, p<0.01), and median total cost of hospitalization ($272,000 vs $45,600, p<0.01) (Figure 1).
Conclusion: Our nationwide study suggests HIT as an independent risk factor for poor hospitalization outcomes including death among patients admitted with COVID-19. Early recognition and prompt cessation of heparin related products can help prevent catastrophic thrombotic complications.
Disclosures
Jaglal:Agios: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; SOBI: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal